
Minimize Complexity,
Maximize Versatility
The entire GMK Total Knee Replacement System has been designed to preserve the joint functionality without dramatically altering its anatomy and kinematics, even in cases of severe ligament instability or massive bone defects.
Thanks to the GMK Revision comprehensive range of options the surgeon can choose the most suitable solution for every patient within his care without any compromise.
The established GMK REVISION implant, along with the easy to use instrumentation, help the surgeon to operate every day in total confidence, flawlessly addressing each surgical scenario, from primary augmentable cases to the most challenging knee revisions: with GMK REVISION any challenge is possible!

The GMK Revision complete product range, including mobile and fixed bearings, offers different levels of constraint:
6 sizes
Anatomical: left and right
Material: Cobalt-Chrome (Co-Cr-Mo ISO 5832-4)
Cemented

6 sizes
Anatomical: left and right
Material: Cobalt-Chrome (Co-Cr-Mo ISO 5832-4)
Cemented

Material: Cobalt-Chrome (Co-Cr-Mo ISO 5832-4) + SensiTiN coating
.jpg)
6 sizes
Anatomical: left and right
Material: Cobalt-Chrome (Co-Cr-Mo ISO 5832-4)
Cemented

Material: Cobalt-Chrome (Co-Cr-Mo ISO 5832-4) + SensiTiN coating
.jpg)
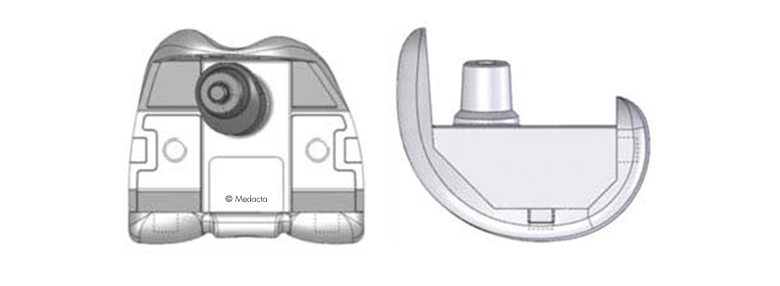
Symmetric, deep dish
Anterior flare to accommodate patellar tendon
6 sizes
5 thickness (10, 12 ,14, 17, 20 mm)
Machined Ultra High Molecular Weight Polyethylene (UHMWPE ISO 5834-2)

Symmetric
Anterior flare to accommodate patellar tendon
6 sizes
5 thickness (10, 12 ,14, 17, 20 mm)
Additional fixation screw
Machined Ultra High Molecular Weight Polyethylene (UHMWPE ISO 5834-2)

Symmetric
Anterior flare to accommodate patellar tendon
6 sizes
5 thickness (10, 12 ,14, 17, 20, 23, 26 mm)
Additional fixation screw
Machined Ultra High Molecular Weight Polyethylene (UHMWPE ISO 5834-2)

Interchangeable femur / tibia
2 offset: 3, 5 mm
Titanium alloy (Ti6Al4V, ISO 5832-3)

Interchangeable femur / tibia
Diameter = 10,11,12,13,14,15,16,18,20,22 mm
Length = 65, 105, 150 mm
Titanium alloy (Ti6Al4V, ISO 5832-3)

Interchangeable femur / tibia
Tapered shape
Diameter = 11, 13, 16 mm
Length = 65, 105 mm
Titanium alloy (Ti6Al4V, ISO 5832-3)

Mechanically attached to femoral component (screw included)
Interchangeable medial / lateral side
Five levels of thickness: 4, 8, 12, 16, 20 mm
High nitrogen Stainless steel (M30NW, ISO 5832-9) and Titanium alloy screw (Ti6Al4V, ISO 5832-3)

Mechanically attached to femoral component (screw included)
Interchangeable medial / lateral side
Two levels of thickness: 5, 10 mm
High nitrogen Stainless steel (M30NW, ISO 5832-9) and Titanium alloy screw (Ti6Al4V, ISO 5832-3)

Mechanically attached to femoral component (screws included)
Interchangeable medial / lateral side
Four levels of thickness: 5, 10, 15, 20 mm
High nitrogen Stainless steel (M30NW, ISO 5832-9) and Titanium alloy screw (Ti6Al4V, ISO 5832-3)

Anatomical shape
4 sizes
Machined Ultra High Molecular Weight Polyethylene (UHMWPE ISO 5834-2)
Cemented
Three fixation pegs

Round shape
3 sizes
Machined Ultra High Molecular Weight Polyethylene (UHMWPE ISO 5834-2)
Cemented
One central fixation peg

The femoral box is reduced to a minimum, saving precious bone stock.
MECHANICAL PROPERTIES
The internal reinforcement metal peg provides further resistance. Mechanical tests show proven stability and mechanical resistance of GMK REVISION semi-constrained inlay*.
POLYETHYLENE
Published papers show that polyethylene that does not undergo any irradiation or thermal treatments, that may affect mechanical properties, may show reduced potential of delamination[1]. Medacta provides machined, non-irradiated polyethylene for all GMK tibial inserts.
The internal surface of the tibial baseplate is mirror polished, minimizing the risk of backside wear.
The keel dimensions are the same as for GMK PRIMARY, allowing for the use of a modular offset.
Cemented augments are available to fill bone defects and manage the joint line position.
Interchangeable modular offset adapters are available for femur and tibia in order to provide the maximum flexibility with the minimum inventory, avoiding the need for additional offseted stems.
All the modular connections are accurately tested* and dedicated instruments are available in the operative room to ensure a reproducbile fixation.
*Data on file: Medacta
To face different clinical indications, both cementless and cemented options are available. Cementless stems have longitudinal splines to provide rotational stability, whereas cemented stems have longitudinal pockets for cement and fluted shape to facilitate insertion.

ADD EASY-TO-USE AND SAFE INSTRUMENTATION TO A VERSATILE RANGE OF PRODUCT: THE RESULT IS GMK REVISION
The primary goal of a GMK Revision knee replacement includes the restoration of anatomical alignment and functional stability, the accurate reestablishment of the joint line and the fixation and stabilization of the revision prosthetic implant components.
The GMK Revision has a flexible instrumentation allowing to follow different surgical techniques, depending on the surgeon's preferences and the clinical circumstances. The surgeon can therefore benefit of the maximum confidence even in the most challenging situation.

Dedicated instruments are provided to precisely reproduce the validated offset on femur and tibia, all the modular connections are then secured by Morse taper and additional screw and provided dynamometric wrenches and special impactors always ensure a standardized and reproducible procedure.

Tibial and femoral resections can be accurately fine-tuned thanks to micrometric systems, in order to preserve as much bone as possible and facilitate the joint line management.

Multiple checks at different operative stages allow to manage the joint line position in order to restore the functionality of the extensor mechanism. Patellar tracking can be adjusted up to the femoral trialing step as femoral augment resections can be performed directly through the trial femur.
Provided instruments allow to easily switch intra-operatively from a less constrained to a more constrained inlay when more stability is required, without the need for huge additional instrumentation.
DESIGN RATIONALE
[1] Ries M D, “Highly Cross-Linked Polyethylene. The Debate is Over-In Opposition”, The Journal of Arthroplasty, 20:59-62, 2005.
[2] Kondo et al. “Arthroscopy for evaluation of polyethylene wear after total knee arthroplasty”, J Orthop Sci, 13:433-437, 2008. Orthop Sci, 13:433-437, 2008
[3] Baker et al., “The effects of degree of Crosslinking on the fatigue crack initiation and propagation resistane of orthopedic-grade polyethylene”, J Biomed Mater Res A, 66(1):146-54, 2002.
[4] Muratoglu et al., “Unified wear model for highly crosslinked ultra-high molecular weight polyethylenes (UHMWPE)”, Biomaterials, 20:1463-70, 1999.
[5] Polyethylene in TKA: Do we really need cross-linked polyethylene?, MORE Journal Vol. 1 May 2011
[6] Anderson MJ, Becker DL, Kieckbusch T. - Patellofemoral complications after posterior-stabilized total knee arthroplasty: a comparison of 2 different implant designs. - J Arthroplasty. 2002 Jun;17(4):422-6
[7] D'Lima DD, Chen PC, Kester MA, Colwell CW Jr. - Impact of patellofemoral design on patellofemoral forces and polyethylene stresses. - J Bone Joint Surg Am. 2003;85-A Suppl 4:85-93.
[8] Morra EA, Greenwald AS. - Patellofemoral replacement polymer stress during daily activities: a finite element study - J Bone Joint Surg Am. 2006 Dec;88 Suppl 4:213-6
[9] Sharma A, Komistek RD, Ranawat CS, Dennis DA, Mahfouz MR - In vivo contact pressures in total knee arthroplasty. - J Arthroplasty. 2007 Apr;22(3):404-16
[10] Baldwin JL, House CK. - Anatomic dimensions of the patella measured during total knee arthroplasty. - J Arthroplasty. 2005 Feb;20(2):250-7.
[11] Kulkarni SK, Freeman MA, Poal-Manresa JC, Asencio JI, Rodriguez JJ. - The patellofemoral joint in total knee arthroplasty: is the design of the trochlea the critical factor? - J Arthroplasty. 2000 Jun;15(4):424-9.
Same internal and articular femoral profiles between GMK REVISION and GMK PRIMARY ensure the freedom to choose intra-operatively the most suitable constraint for the patient, even after the bone cuts being performed.
Moreover, the wide compatibility with the primary polyethylene inlays as well the use of the same primary tibial component allow the hospital to save stock inventory.
